Brain-controlled Robotic Exoskeletons
Keith Thompson doesn’t remember the night that left him paralyzed.
As a police officer, he was called to assist in the pursuit of a stolen vehicle. The car thief T-boned the police cruiser Thompson was driving and sent Thompson’s car spinning into a tree.
“I never once thought of it happening to me,” he said, “and it did.”
Thompson suffered extensive brain injuries and was comatose for almost three weeks following the accident, but it wasn’t impact that put him in a wheelchair. It was the necessary, life-saving actions of the medical team to repair his ruptured aorta that cut off blood supply to the spine and left the lower half of his body paralyzed. Thompson said he’s glad the team did what they could to save his life.
He has an incomplete spinal cord injury, so Thompson still has partial feeling from the waist to the knees. He can still control movement in his hips, but not his legs. Thompson has now been in a wheelchair for for almost 18 years and continues to do physical therapy several times each week.
“I just want to have my body ready for the cure,” Thompson said. “Why sit around doing nothing? When they do come out with a cure, my legs will be ready for it, my body will.”
Thompson had been a police officer in Omaha, Neb., for five years before the accident occurred in August 1996. He returned to the police department about a year after the crash and continues to work in the Information Services Unit, responding to calls from the community and addressing non-emergency concerns.
Thompson is one of about six million people living with paralysis in the United States. An estimated 12,000 spinal cord injuries occur every year, according to the National Institutes of Health.
Researchers are looking for solutions to help people regain use of their limbs. In a healthy nervous system, signals are sent from the brain, down the spinal cord and out to the peripheral nerves in the muscles to initiate movement. A spinal cord injury disrupts this pathway. One solution is to create new pathways for signals to travel either directly to the muscles or to a mechanical device, bypassing the injured spinal cord.
In this way, amputees can operate a prosthetic limb or paralyzed patients can walk using a robotic suit. ‘Brain-machine interface’ is the buzzword in the field, referring to electrical signals from the brain connecting to a mechanical device that initiates movement. In other cases, the brain-machine interface carries those brain signals to targeted muscles.
While researchers have made great progress in brain science over the years, they still have many mysteries to uncover. Daofen Chen, a program officer for the National Institute of Neurological Disorders and Stroke, said the recent surge of brain-machine interfaces has succeeded because computer science and engineering technology have gotten more sophisticated, not because scientists necessarily know more about the brain.
Chen said he didn’t want to downplay recent advances in neuroscience, but he said “In comparison, the critical, game-changing part of it is really the technology.”
Reading the brain: gathering and processing signals
In order for devices controlled by a brain-machine interface to work, scientists must successfully acquire and decode a person’s brain signals. The technology can vary, but all systems require sensors to measure brain activity.
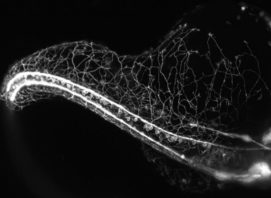
The brain has billions of neurons, and it’s impossible for scientists to collect signals from them all at once. Luckily, only a small fraction of the brain’s neurons need to activate to create signals that lead to physical movements.
“Typically in these experiments we record 100 to 200 neurons,” said Lee Miller, a researcher and professor at Northwestern University, “which sounds funny to say, but are more than are needed to specify the movement.”
Researchers are looking at brain activity trying to predict what the brain is telling the body to do. In ongoing experimental work, scientists record signals from patients as they perform movements, like walking. They simultaneously record what the brain is doing and what the body is doing, so they can later match up the brain signals to same movement. For paralyzed patients who cannot walk, scientists collect patients’ brain signals as they simply think about walking. Using the data, researchers can develop algorithms that predict the most likely movement the brain is calling for.
Some methods for collecting brain signals are considered invasive —meaning they require surgery— while others are not.
In 2012, Miller used electrodes implanted directly on the surface of the brain to move a monkey’s paralyzed hand.
“Muscles can be made to contract by stimulating with electricity,” Miller said. “What we did on top of that was very carefully controlled the level of that electrical stimulation, so the muscle contracted with precisely the amount of force that we wanted.”
Implanted microelectrodes in the brain collect more precise data of rapidly firing neural signals, compared to a non-invasive approach, because the electrodes directly touch the neurons. But the need for surgery makes implants a riskier endeavor, and researchers have yet to develop an implantable, wireless system. At present, implanted electrodes are connected to wires outside of the body, leading to risk of infection.
“With these very early neural prosthetic implants, there’s a connector that sticks out of the head,” said Joseph O’Doherty, a researcher at the University of California, San Francisco. We’re not really meant to have things poke through our skin, so that’s a huge risk right there.”
Miller said placing a foreign object in the body is not a good long-term solution as the implant generates scar tissue around the electrode. These electrodes would have to be surgically replaced every couple years, and a new location in the brain determined each time.
“We need electrode arrays that will last for decades rather than years,” Miller said. “That’s, I think, the fundamental limitation for all brain-machine interfaces.”
Because of the risks and limitations of the implanted electrodes, some researchers are using non-invasive methods for gathering brain signals.
Researchers at the University of Houston use electroencephalography (EEG) to measure brain activity. The user wears a skullcap of precisely placed sensors, like a swimming cap, on the outside of the body.
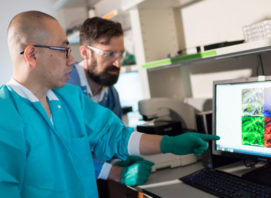
Using the EEG recording, patients have been able to control robotic exoskeleton devices. The exoskeleton is a wearable robotic suit that users put over their clothes—think a less sophisticated Iron Man suit. Researchers in the Laboratory for Non-Invasive Brain-Machine Interfaces, led by Jose Contreras-Vidal, design and test non-invasive brain-machine interface systems for patients living with the effects of stroke, spinal cord injury and amputation.
Atilla Kilicarslan, a research associate in the lab, works with NeuroREX, an adapted Rex Bionics device. The Rex Bionics exoskeleton was developed by researchers in New Zealand to help paralyzed people walk and is operated using hand controls similar to a wheelchair. The device is self-supporting, so the user doesn’t need crutches or other assistance to maintain balance.
Kilicarslan makes sure the robot is maintained and in working order for the patient trials. The hulking device must be measured to fit the patient’s height, and Kilicarslan emphasized the need for accuracy to ensure patient safety. The NeuroREX acts as a puppeteer, moving the patient’s legs because they can’t move on their own. If not fitted properly, the metal device could strain the body or even snap a leg bone.
The Houston group is working to adapt the control system so the NeuroREX can be controlled by the user’s thoughts. Kilicarslan writes the algorithms that make this communication between brain and robot possible.
“All they need to do is think about moving forward,” Kilicarslan said. “We don’t ask them to imagine anything in particular. So far the hardest part technically is to capture that intention each and every time the user is trying to move forward.”
Steve Holbert, a patient volunteer who has been paralyzed for four years, said learning to use the NeuroREX device was fairly intuitive.
“The signal is instantaneous and the computer program is relatively fast so it’s quick enough,” Holbert said. While the brain signals are gathered by the EEG and quickly decoded, the robot doesn’t always respond to commands quickly, with users sometimes experiencing a few seconds delay.
Contreras-Vidal said there is room for improvement. “A 99 percent success rate is not good enough,” he said. “A spinal cord injured patient would not want a neuroprosthetic device that fails every 99 out of 100 steps.”
Building on movement: Adding sensory feedback
While brain-machine interface devices focus on restoring movement to those who have lost it partially or completely, paralyzed people also lack tactile feedback, or a sense of touch, that helps them better navigate their environment.
“A good example is when you pick up a cup of coffee,” O’Doherty said. “You’re going to want to know how to grasp it enough that it doesn’t fall out and smash on the floor, or squeeze it so hard that it crushes it.”
O’Doherty created an invasive brain-machine-brain interface for sensory feedback during his graduate studies in the Nicolelis Lab at the Duke University Medical Center. It’s called a brain-machine-brain interface because the brain starts by sending signals to a device. Sensors also send signals back to the brain, letting the brain know when the individual touched an object. The device creates a loop of the brain both sending and receiving signals, enabling the individual to better adapt to the environment.
O’Doherty’s work involved a virtual environment with monkeys interacting with objects on a computer screen. As the monkeys moved a computer cursor on a screen using their brain signals, the monkeys could “touch” the virtual objects they saw.
Much of the brain-machine interface work has focused on restoring movement, which is very important but, as O’Doherty said, only part of the equation.
“If you think about it, when your limbs are numb, you’re not going to move normally,” O’Doherty said. “When you receive feedback on what you’re doing, it helps you make better movements.”
Hope for the future
Further neuroscience research can lead to a better understanding of how the brain works that, in turn, can improve the functionality of brain-machine interfaces.
Police officer Keith Thompson said he hopes his long-term paralysis won’t prevent him from benefitting from progress in the field.
“I feel like they might focus on newly injured people,” Thompson said, “and I want to know what they’ll have for the guys who have been in the chair for a long time.”
Although those in the immediate period following a spinal cord injury have a better chance of rewiring their nervous systems, Contreras-Vidal sais brain-machine interfaces, in principle, could also help those with long-term paralysis.
Over the last 18 years, Thompson has tried several therapies.
“You can’t ever give up,” he said. “There’s a reason why God does things, and I just think he’s given me the motivation and the discipline to keep going. So I am going.”